
原文引自微信公众号:ICL技术培训中国 3月5日导语 干眼病(DED)是一种多因素的眼表疾病,其特征是泪膜内稳态丧失,并伴有眼部症状,病因包括泪膜不稳定和泪液高渗透压、眼表炎症和损伤以及神经感觉异常5。另外,干眼病也可能是由医源性干预措施引起,包括全身或局部药物,隐形眼镜,眼科手术(例如角膜屈光手术和白内障手术)8等。 干眼病是LASIK手术后最常报告的问题11,12。ICL术后偶见干眼报道,但因为ICL手术与白内障或屈光性晶状体置换术(RLE)的相似性,可能也存在一些相同的干眼危险因素8。但大部分记录了激光视力矫正(LVC)手术或ICL手术后干眼症状的文章观察时间有限,没有研究评估屈光手术后长达5年或更长时间的干眼症状。 因此,挪威东南大学团队进行了相关研究,比较5到15年前接受LVC或ICL的患者与没有屈光手术史的类似人群的干眼病体征以及干眼病的患病率,该研究结果于2020年发表在Clinical Ophthalmology。研究设计 这是一项横断面病例对照研究。研究纳入共257名受试者,包括5 - 15年前接受LVC(LASIK或Femto-LASIK)手术或ICL(V4型)手术的患者和对照组,对照组为无屈光手术史的年龄匹配组,随机选择一只测试眼。采用泪液渗透压(双眼测量)、眼表疾病指数(OSDI)、客观散射指数(OSI)、非侵入性泪膜破裂时间(NIKBUT)、睑板腺照相和SchirmerⅠ试验等标准评估干眼病。研究结果 研究共纳入257位患者:LVC组94位(45位女性,49位男性),ICL组80位(57位女性,23位男性),对照组83位(41位女性,42位男性)。 与LVC组相比,ICL组的女性患者明显多于对照组,并且手术后的时间明显更长。两组之间的术前验光存在显着差异。(表1)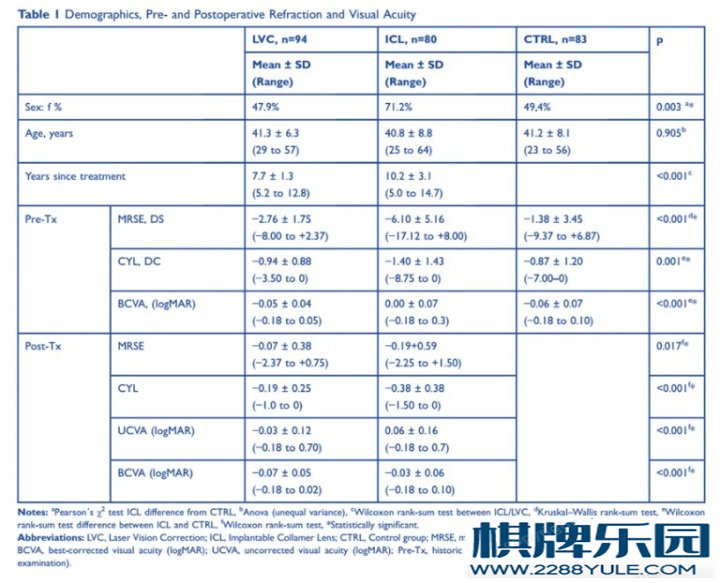 LVC组的高泪液渗透压的比例明显高于对照组(73%vs 50%,p = 0.002)。相反,LVC组的主观症状发生率往往低于对照组(19%对比31%;p = 0.06)。在ICL和对照组之间未发现这些差异。ICL组的VBUT≤10 s的频率明显高于对照组(33%vs 17%)。(表3,图1) LVC组的高泪液渗透压的比例明显高于对照组(73%vs 50%,p = 0.002)。相反,LVC组的主观症状发生率往往低于对照组(19%对比31%;p = 0.06)。在ICL和对照组之间未发现这些差异。ICL组的VBUT≤10 s的频率明显高于对照组(33%vs 17%)。(表3,图1)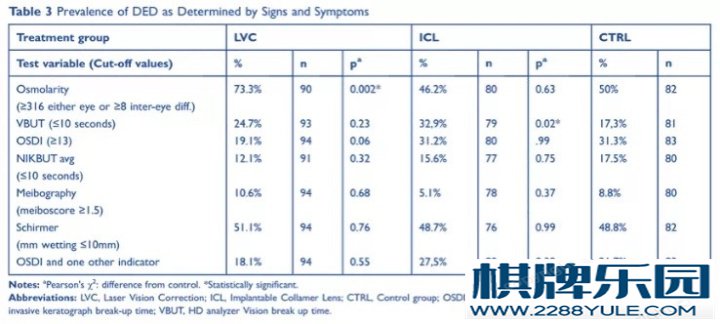 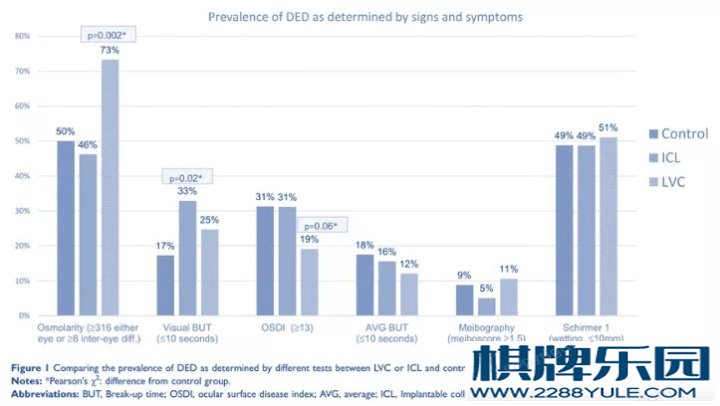 讨论 研究发现,LVC组的高泪液渗透压的比例明显高于对照组和ICL组。这可能是由于泪液渗透压的差异性是DED的标志42。在所有组中,DED的患病率较高可能是因为,当患者因干眼而导致不能佩戴隐形眼镜时,更可能考虑接受屈光手术作为解决方案。据报道,多达73%的LVC患者寻求手术是因为隐形眼镜配戴困难14,45。另外,年龄是DED的危险因素,本研究中,LVC和ICL组患者的平均年龄分别比手术时大8岁和10岁6。 LVC组的主观症状倾向于减少。研究表明,由于年龄,耐受性,环境甚至是长期干眼的差异,主观和客观症状可能会不一致,这会降低患者的敏感性3,43。在LASIK术后患者中,症状减轻可能是由于敏感性降低所致。Take home message:ICL不增加术后干眼症状 与无屈光手术史的年龄匹配对照组相比,ICL术后5-15年的患者的高泪液渗透压的比例和DED主观症状发生率均无明显差异。LVC术后5-15年的患者高泪液渗透压的比例明显高于对照组,干眼病主观症状发生率低于对照组,可能与主观症状的敏感性降低有关。文献来源:http://doi.org/10.2147/OPTH.S236749参考文献:1. Haigis W. Intraocular lens calculation after refractive surgery for myopia: haigis-L formula. J Cataract Refract Surg. 2008;34 (10):1658–1663. doi:10.1016/j.jcrs.2008.06.0292. Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85(5):472–485. doi:10.1111/j.1755-3768.2007.00879.x3. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41(8):1672–1677. doi:10.1016/j.jcrs.2015.01.0164. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.0085. Nelson JD, Craig JP, Akpek EK, et al. TFOS DEWS II introduction. Ocul Surf. 2017;15(3):269–275. doi:10.1016/j.jtos.2017.05.0056. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438–510. doi:10.1016/j.jtos.2017.05.0117. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539–574. doi:10.1016/j.jtos.2017.05.0018. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511–538. doi:10.1016/j.jtos.2017.05.0049. Solomon KD, Fernandez de Castro LE, Sandoval HP, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691–701. doi:10.1016/j.ophtha.2008.12.03710. Statista. Number of LASIK surgeries in the United States from 1996 to 2020. Statista; 2019. Available from: https://www.statista.com/statistics/271478/number-of-lasik-surgeries-in-the-us/. Accessed December 08, 2019.11. Solomon R, Donnenfeld ED, Perry HD. The effects of LASIK on the ocular surface. Ocul Surf. 2004;2(1):34–44. doi:10.1016/S1542-0124(12)70022-812. Ambrósio R, Tervo T, Wilson SE. LASIK-associated dry eye and neurotrophic epitheliopathy: pathophysiology and strategies for prevention and treatment. J Refract Surg. 2008;24(4):396–407. doi:10.3928/1081597X-20080401-1413. Xie W. Recent advances in laser in situ keratomileusis-associated dry eye. Clin Exp Optom. 2016;99(2):107–112. doi:10.1111/cxo.1236114. Cohen E, Spierer O. Dry eye post-laser-assisted in situ keratomileusis: major review and latest updates. J Ophthalmol. 2018;2018:4903831.15. Wilson SE, Ambrósio R. Laser in situ keratomileusis-induced neurotrophic epitheliopathy. Am J Ophthalmol. 2001;132(3):405. doi:10.1016/S0002-9394(01)00995-316. Feng YF, Yu JG, Wang DD, et al. The effect of hinge location on corneal sensation and dry eye after LASIK: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2013;251(1):357–366.17. Lee JB, Ryu CH, Kim J-H, Kim EK, Kim HB. Comparison of tear secretion and tear film instability after photorefractive keratectomy and laser in situ keratomileusis1. J Cataract Refract Surg. 2000;26(9):1326–1331. doi:10.1016/S0886-3350(00)00566-618. Nettune GR, Pflugfelder SC. Post-LASIK tear dysfunction and dysesthesia. Ocul Surf. 2010;8(3):135–145. doi:10.1016/S1542-0124(12)70224-019. Shoja MR, Besharati MR. Dry eye after LASIK for myopia: incidence and risk factors. Eur J Ophthalmol. 2007;17(1):1–6. doi:10.1177/11206721070170010120. De Paiva CS, Chen Z, Koch DD, et al. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol. 2006;141(3):438–445. doi:10.1016/j.ajo.2005.10.00621. Dooley I, D’Arcy F, O’Keefe M. Comparison of dry-eye disease severity after laser in situ keratomileusis and laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2012;38(6):1058–1064. doi:10.1016/j.jcrs.2012.01.02822. Wang X, Zhou X. Update on treating high myopia with implantable collamer lenses. Asia Pac J Ophthalmol (Phila). 2016;5(6):445–449. doi:10.1097/APO.000000000000023523. Dougherty PJ, Priver T. Refractive outcomes and safety of the implantable collamer lens in young low-to-moderate myopes. Clin Ophthalmol. 2017;11:273–277. doi:10.2147/OPTH24. Naj AC, Liang G-L, Wu J, et al. Implantable collamer lens versus iris-fixed phakic intraocular lens implantation to correct myopia: a meta-analysis. PLoS One. 2014;9(8):e104649.25. TearLab. Osmolarity System - User Manual. San Diego, CA: U.S.A. TearLab Corporation; 2017.26. Gouvea L, Waring IGO, Brundrett A, Crouse M, Rocha KM. Objective assessment of optical quality in dry eye disease using a double-pass imaging system. Clin Ophthalmol. 2019;13:1991–1996. doi:10.2147/OPTH.S21158427. Herbaut A, Liang H, Rabut G, et al. Impact of dry eye disease on vision quality: an optical quality analysis system study. Transl Vis Sci Technol. 2018;7(4):5. doi:10.1167/tvst.7.4.528. Monte´s-Mico´ R, Alio´ JL, Charman WN. Postblink changes in the ocular modulation transfer function measured by a double-pass method. Invest Ophthalmol Vis Sci. 2005;46(12):4468–4473. doi:10.1167/iovs.05-060929. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615–621. doi:10.1001/archopht.118.5.61530. Oculus. Oculus Keratograph 5M User Guide. Wetzlar, Germany: Oculus Optikergerâte; 2017.31. Oculus. Oculus Keratograph 5M Instruction Manual. Wetzlar, Germany: Oculus Optikgeräte; 2017.32. Savini G. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008;31.33. Best N, Drury L, Wolffsohn JS. Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye. 2012;35(4):171–174. doi:10.10 16/j.clae.2012.04.00234. Tian L, Qu JH, Zhang XY, Sun XG. Repeatability and reproducibility of noninvasive keratograph 5M measurements in patients with dry eye disease. J Ophthalmol. 2016;2016:8013621.35. Jiang Y, Ye H, Xu J, Lu Y. Noninvasive Keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res. 2014;42(2):494–502. doi:10.1177/030006051350470136. Arita R, Itoh K, Maeda S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009;11(11):2058–2063. doi:10.1016/j.ophtha.2009.04.03737. Finis D, Ackermann P, Pischel N, et al. Evaluation of meibomian gland dysfunction and local distribution of meibomian gland atrophy by non-contact infrared meibography. Curr Eye Res. 2015;40(10):982–989. doi:10.3109/02713683.2014.97192938. de Monchy I, Gendron G, Miceli C, Pogorzalek N, Mariette X, Labetoulle M. Combination of the Schirmer I and phenol red thread tests as a rescue strategy for diagnosis of ocular dryness associated with sjögren’s syndrome. Invest Ophthalmol Vis Sci. 2011;52(8):5167–5173. doi:10.1167/iovs.10-667139. Hill WE, Wang L, Koch DD IOL power calculation in eyes that have undergone LASIK/PRK/RK, online calculator, version 4.9. Available from: http://iolcalc.ascrs.org/. Accessed December 10, 2019.40. Vrijman V, Abulafia A, van der Linden JW, van der Meulen IJE, Mourits MP, Lapid-Gortzak R. Evaluation of different IOL calculation formulas of the ASCRS calculator in eyes after corneal refractive laser surgery for myopia with multifocal IOL implantation. J Refract Surg. 2019;35(1):54–59. doi:10.3928/1081597X-20181119-0141. Brenner LF, Gjerdrum B, Aakre BM, Lundmark PO, Nistad K. Presbyopic refractive lens exchange with trifocal intraocular lens implantation after corneal laser vision correction: refractive results and biometry analysis of 241 eyes. J Cataract Refract Surg. 2019;45:1404–1415. doi:10.1016/j.jcrs.2019.05.03142. Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol.2011;151(5):792–798. doi:10.1016/j.ajo.2010.10.03243. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.00344. Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44 (9):1090–1096. doi:10.1016/j.jcrs.2018.06.02645. McGhee CN, Orr D, Kidd B, Stark C, Bryce IG, Anastas CN. Psychological aspects of excimer laser surgery for myopia: reasons for seeking treatment and patient satisfaction. Br J Ophthalmol. 1996;80(10):874. doi:10.1136/bjo.80.10.87446. Toda I, Asano-Kato N, Hori-Komai Y, Tsubota K. Laser-assisted in situ keratomileusis for patients with dry eye. JAMA Ophthalmol. 2002;120(8):1024–1028.47. Konomi K, Chen LL, Tarko RS, et al. Preoperative characteristics and a potential mechanism of chronic dry eye after LASIK. Invest Ophthalmol Vis Sci. 2008;49(1):168–174. doi:10.1167/iovs.07-033748. Artigas JM, Peris C, Felipe A, Menezo JL, Sanchez-Cortina I, LopezGil N. Modulation transfer function: rigid versus foldable phakic intraocular lenses. J Cataract Refract Surg. 2009;35(4):747–752. doi:10.1016/j.jcrs.2008.12.02049. Shtein RM. Post-LASIK dry eye. Expert Rev Ophthalmol. 2011;6 (5):575–582. doi:10.1586/eop.11.5650. Potvin R, Makari S, Rapuano C. Tear film osmolarity and dry eye disease: a review of the literature. Clin Ophthalmol. 2015;2039. doi:10.2147/OPTH51. Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2014;92(2):161–166. doi:10.1111/aos.12012 讨论 研究发现,LVC组的高泪液渗透压的比例明显高于对照组和ICL组。这可能是由于泪液渗透压的差异性是DED的标志42。在所有组中,DED的患病率较高可能是因为,当患者因干眼而导致不能佩戴隐形眼镜时,更可能考虑接受屈光手术作为解决方案。据报道,多达73%的LVC患者寻求手术是因为隐形眼镜配戴困难14,45。另外,年龄是DED的危险因素,本研究中,LVC和ICL组患者的平均年龄分别比手术时大8岁和10岁6。 LVC组的主观症状倾向于减少。研究表明,由于年龄,耐受性,环境甚至是长期干眼的差异,主观和客观症状可能会不一致,这会降低患者的敏感性3,43。在LASIK术后患者中,症状减轻可能是由于敏感性降低所致。Take home message:ICL不增加术后干眼症状 与无屈光手术史的年龄匹配对照组相比,ICL术后5-15年的患者的高泪液渗透压的比例和DED主观症状发生率均无明显差异。LVC术后5-15年的患者高泪液渗透压的比例明显高于对照组,干眼病主观症状发生率低于对照组,可能与主观症状的敏感性降低有关。文献来源:http://doi.org/10.2147/OPTH.S236749参考文献:1. Haigis W. Intraocular lens calculation after refractive surgery for myopia: haigis-L formula. J Cataract Refract Surg. 2008;34 (10):1658–1663. doi:10.1016/j.jcrs.2008.06.0292. Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85(5):472–485. doi:10.1111/j.1755-3768.2007.00879.x3. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41(8):1672–1677. doi:10.1016/j.jcrs.2015.01.0164. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.0085. Nelson JD, Craig JP, Akpek EK, et al. TFOS DEWS II introduction. Ocul Surf. 2017;15(3):269–275. doi:10.1016/j.jtos.2017.05.0056. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438–510. doi:10.1016/j.jtos.2017.05.0117. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539–574. doi:10.1016/j.jtos.2017.05.0018. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511–538. doi:10.1016/j.jtos.2017.05.0049. Solomon KD, Fernandez de Castro LE, Sandoval HP, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691–701. doi:10.1016/j.ophtha.2008.12.03710. Statista. Number of LASIK surgeries in the United States from 1996 to 2020. Statista; 2019. Available from: https://www.statista.com/statistics/271478/number-of-lasik-surgeries-in-the-us/. Accessed December 08, 2019.11. Solomon R, Donnenfeld ED, Perry HD. The effects of LASIK on the ocular surface. Ocul Surf. 2004;2(1):34–44. doi:10.1016/S1542-0124(12)70022-812. Ambrósio R, Tervo T, Wilson SE. LASIK-associated dry eye and neurotrophic epitheliopathy: pathophysiology and strategies for prevention and treatment. J Refract Surg. 2008;24(4):396–407. doi:10.3928/1081597X-20080401-1413. Xie W. Recent advances in laser in situ keratomileusis-associated dry eye. Clin Exp Optom. 2016;99(2):107–112. doi:10.1111/cxo.1236114. Cohen E, Spierer O. Dry eye post-laser-assisted in situ keratomileusis: major review and latest updates. J Ophthalmol. 2018;2018:4903831.15. Wilson SE, Ambrósio R. Laser in situ keratomileusis-induced neurotrophic epitheliopathy. Am J Ophthalmol. 2001;132(3):405. doi:10.1016/S0002-9394(01)00995-316. Feng YF, Yu JG, Wang DD, et al. The effect of hinge location on corneal sensation and dry eye after LASIK: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2013;251(1):357–366.17. Lee JB, Ryu CH, Kim J-H, Kim EK, Kim HB. Comparison of tear secretion and tear film instability after photorefractive keratectomy and laser in situ keratomileusis1. J Cataract Refract Surg. 2000;26(9):1326–1331. doi:10.1016/S0886-3350(00)00566-618. Nettune GR, Pflugfelder SC. Post-LASIK tear dysfunction and dysesthesia. Ocul Surf. 2010;8(3):135–145. doi:10.1016/S1542-0124(12)70224-019. Shoja MR, Besharati MR. Dry eye after LASIK for myopia: incidence and risk factors. Eur J Ophthalmol. 2007;17(1):1–6. doi:10.1177/11206721070170010120. De Paiva CS, Chen Z, Koch DD, et al. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol. 2006;141(3):438–445. doi:10.1016/j.ajo.2005.10.00621. Dooley I, D’Arcy F, O’Keefe M. Comparison of dry-eye disease severity after laser in situ keratomileusis and laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2012;38(6):1058–1064. doi:10.1016/j.jcrs.2012.01.02822. Wang X, Zhou X. Update on treating high myopia with implantable collamer lenses. Asia Pac J Ophthalmol (Phila). 2016;5(6):445–449. doi:10.1097/APO.000000000000023523. Dougherty PJ, Priver T. Refractive outcomes and safety of the implantable collamer lens in young low-to-moderate myopes. Clin Ophthalmol. 2017;11:273–277. doi:10.2147/OPTH24. Naj AC, Liang G-L, Wu J, et al. Implantable collamer lens versus iris-fixed phakic intraocular lens implantation to correct myopia: a meta-analysis. PLoS One. 2014;9(8):e104649.25. TearLab. Osmolarity System - User Manual. San Diego, CA: U.S.A. TearLab Corporation; 2017.26. Gouvea L, Waring IGO, Brundrett A, Crouse M, Rocha KM. Objective assessment of optical quality in dry eye disease using a double-pass imaging system. Clin Ophthalmol. 2019;13:1991–1996. doi:10.2147/OPTH.S21158427. Herbaut A, Liang H, Rabut G, et al. Impact of dry eye disease on vision quality: an optical quality analysis system study. Transl Vis Sci Technol. 2018;7(4):5. doi:10.1167/tvst.7.4.528. Monte´s-Mico´ R, Alio´ JL, Charman WN. Postblink changes in the ocular modulation transfer function measured by a double-pass method. Invest Ophthalmol Vis Sci. 2005;46(12):4468–4473. doi:10.1167/iovs.05-060929. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615–621. doi:10.1001/archopht.118.5.61530. Oculus. Oculus Keratograph 5M User Guide. Wetzlar, Germany: Oculus Optikergerâte; 2017.31. Oculus. Oculus Keratograph 5M Instruction Manual. Wetzlar, Germany: Oculus Optikgeräte; 2017.32. Savini G. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008;31.33. Best N, Drury L, Wolffsohn JS. Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye. 2012;35(4):171–174. doi:10.10 16/j.clae.2012.04.00234. Tian L, Qu JH, Zhang XY, Sun XG. Repeatability and reproducibility of noninvasive keratograph 5M measurements in patients with dry eye disease. J Ophthalmol. 2016;2016:8013621.35. Jiang Y, Ye H, Xu J, Lu Y. Noninvasive Keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res. 2014;42(2):494–502. doi:10.1177/030006051350470136. Arita R, Itoh K, Maeda S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009;11(11):2058–2063. doi:10.1016/j.ophtha.2009.04.03737. Finis D, Ackermann P, Pischel N, et al. Evaluation of meibomian gland dysfunction and local distribution of meibomian gland atrophy by non-contact infrared meibography. Curr Eye Res. 2015;40(10):982–989. doi:10.3109/02713683.2014.97192938. de Monchy I, Gendron G, Miceli C, Pogorzalek N, Mariette X, Labetoulle M. Combination of the Schirmer I and phenol red thread tests as a rescue strategy for diagnosis of ocular dryness associated with sjögren’s syndrome. Invest Ophthalmol Vis Sci. 2011;52(8):5167–5173. doi:10.1167/iovs.10-667139. Hill WE, Wang L, Koch DD IOL power calculation in eyes that have undergone LASIK/PRK/RK, online calculator, version 4.9. Available from: http://iolcalc.ascrs.org/. Accessed December 10, 2019.40. Vrijman V, Abulafia A, van der Linden JW, van der Meulen IJE, Mourits MP, Lapid-Gortzak R. Evaluation of different IOL calculation formulas of the ASCRS calculator in eyes after corneal refractive laser surgery for myopia with multifocal IOL implantation. J Refract Surg. 2019;35(1):54–59. doi:10.3928/1081597X-20181119-0141. Brenner LF, Gjerdrum B, Aakre BM, Lundmark PO, Nistad K. Presbyopic refractive lens exchange with trifocal intraocular lens implantation after corneal laser vision correction: refractive results and biometry analysis of 241 eyes. J Cataract Refract Surg. 2019;45:1404–1415. doi:10.1016/j.jcrs.2019.05.03142. Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol.2011;151(5):792–798. doi:10.1016/j.ajo.2010.10.03243. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.00344. Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44 (9):1090–1096. doi:10.1016/j.jcrs.2018.06.02645. McGhee CN, Orr D, Kidd B, Stark C, Bryce IG, Anastas CN. Psychological aspects of excimer laser surgery for myopia: reasons for seeking treatment and patient satisfaction. Br J Ophthalmol. 1996;80(10):874. doi:10.1136/bjo.80.10.87446. Toda I, Asano-Kato N, Hori-Komai Y, Tsubota K. Laser-assisted in situ keratomileusis for patients with dry eye. JAMA Ophthalmol. 2002;120(8):1024–1028.47. Konomi K, Chen LL, Tarko RS, et al. Preoperative characteristics and a potential mechanism of chronic dry eye after LASIK. Invest Ophthalmol Vis Sci. 2008;49(1):168–174. doi:10.1167/iovs.07-033748. Artigas JM, Peris C, Felipe A, Menezo JL, Sanchez-Cortina I, LopezGil N. Modulation transfer function: rigid versus foldable phakic intraocular lenses. J Cataract Refract Surg. 2009;35(4):747–752. doi:10.1016/j.jcrs.2008.12.02049. Shtein RM. Post-LASIK dry eye. Expert Rev Ophthalmol. 2011;6 (5):575–582. doi:10.1586/eop.11.5650. Potvin R, Makari S, Rapuano C. Tear film osmolarity and dry eye disease: a review of the literature. Clin Ophthalmol. 2015;2039. doi:10.2147/OPTH51. Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2014;92(2):161–166. doi:10.1111/aos.12012
打麻将技巧十句口诀虽然听起来有些略微官方和不熟悉,但想必这对常年喜欢玩麻将的朋友们来说并不陌生,虽然在叫法上可以稍微会有一些不一致的地方,但殊途同归讲的本质意思还是很一致的,介绍的都是在打麻将过程之中会用到的一些基本技巧和方法,目的就是帮助你在本轮游戏中更快、更准、更稳的取得胜利。这十句口诀往往涵盖了打麻将过程中会遇到的各类容易发生的情况,以及在这种情况下我们需要如何做才能让自己比对手更有把握的胜出。 打麻将技巧十句口诀中,“三狠四杀;也是经常用到。所谓的“狠;就是出牌要狠,也就是说不要犹豫。当然这也是有前提的,玩家们需要有精准的出牌判断棋牌问答,该出牌的时候就出牌,不要因为自己的犹豫而最后一败涂地。而“杀;就是要不要因为同情而一时的手软,看清楚自己的牌局后就下手,形成自己的出牌优势,最终和局。 |